Artificial bone marrow may be used to reproduce hematopoietic stem cells. A prototype has now been developed by scientists of KIT, the Max Planck Institute for Intelligent Systems, Stuttgart, and Tübingen University. The porous structure possesses essential properties of natural bone marrow and can be used for the reproduction of stem cells at the laboratory. This might facilitate the treatment of leukemia in a few years.
The researchers are now presenting their work in the journal Biomaterials.
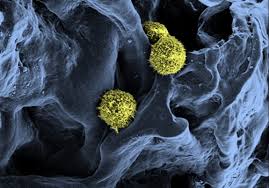
Blood cells, such as erythrocytes or immune cells, are continuously replaced by new ones supplied by hematopoietic stem cells located in a specialized niche of the bone marrow. Hematopoietic stem cells can be used for the treatment of blood diseases, such as leukemia. The affected cells of the patient are replaced by healthy hematopoietic stem cells of an eligible donor.
However, not every leukemia patient can be treated in this way, as the number of appropriate transplants is not sufficient. This problem might be solved by the reproduction of hematopoietic stem cells. So far, this has been impossible, as these cells retain their stem cell properties in their natural environment only, i.e. in their niche of the bone marrow. Outside of this niche, the properties are modified. Stem cell reproduction therefore requires an environment similar to the stem cell niche in the bone marrow.
The stem cell niche is a complex microscopic environment having specific properties. The relevant areas in the bone are highly porous and similar to a sponge. This three-dimensional environment does not only accommodate bone cells and hematopoietic stem cells but also various other cell types with which signal substances are exchanged. Moreover, the space among the cells has a matrix that ensures a certain stability and provides the cells with points to anchor. In the stem cell niche, the cells are also supplied with nutrients and oxygen.
The Young Investigators Group “Stem Cell-Material Interactions” headed by Dr. Cornelia Lee-Thedieck consists of scientists of the KIT Institute of Functional Interfaces (IFG), the Max Planck Institute for Intelligent Systems, Stuttgart, and Tübingen University. It artificially reproduced major properties of natural bone marrow at the laboratory. With the help of synthetic polymers, the scientists created a porous structure simulating the sponge-like structure of the bone in the area of the blood-forming bone marrow. In addition, they added protein building blocks similar to those existing in the matrix of the bone marrow for the cells to anchor.
The scientists also inserted other cell types from the stem cell niche into the structure in order to ensure substance exchange.
Then, the researchers introduced hematopoietic stem cells isolated from cord blood into this artificial bone marrow. Subsequent breeding of the cells took several days. Analyses with various methods revealed that the cells really reproduce in the newly developed artificial bone marrow. Compared to standard cell cultivation methods, more stem cells retain their specific properties in the artificial bone marrow.
The newly developed artificial bone marrow that possesses major properties of natural bone marrow can now be used by the scientists to study the interactions between materials and stem cells in detail at the laboratory. This will help to find out how the behavior of stem cells can be influenced and controlled by synthetic materials. This knowledge might contribute to producing an artificial stem cell niche for the specific reproduction of stem cells and the treatment of leukemia in ten to fifteen years from now.
Source: Science daily



&cropxunits=635&cropyunits=681&format=jpg&quality=90)