Children, even those without severe medical conditions, can die from the flu in as little as three days after symptoms appear, U.S. health officials warn.
Between 2004 and 2012, flu complications killed 830 children in the United States, many of whom were otherwise healthy, according to the U.S. Centers for Disease Control and Prevention.
Most striking is that 35 percent of these children died before being hospitalized or within the first three days of developing symptoms, according to the report published online Oct. 28 in Pediatrics.
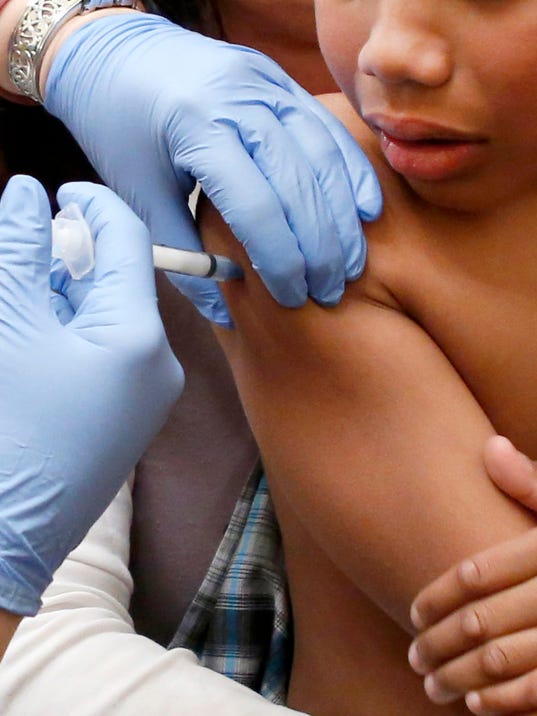
“We found these influenza-related deaths can occur in children with and without medical conditions and in children of all ages, and that very few of these children have been vaccinated,” said lead author Dr. Karen Wong, a CDC medical epidemiologist.
Researchers who reviewed those deaths found that only 22 percent with a high-risk medical condition and just 9 percent without a significant medical condition had been vaccinated.
Wong doesn’t know why so many children die so fast. “About a third of these children die within the first three days of their first reported symptoms,” she said.
One expert wasn’t surprised that many otherwise healthy children who died did so before being admitted to the hospital.
“First, parents don’t realize that flu can be fatal,” said Dr. Marcelo Laufer, a pediatric infectious diseases specialist at Miami Children’s Hospital.
Second, parents of children with chronic diseases “know the system better, so they come earlier than healthy patients,” he said.
Because flu can progress so quickly, prevention is really the best strategy, Wong said. “And that’s why we recommend every child 6 months or older get vaccinated every year,” she said.
Because an infant under 6 months of age can’t be given flu vaccine, Wong said it is vital that pregnant women get a flu shot to help protect their newborn, and that everyone likely to be near the baby also be vaccinated so they can’t pass flu to the infant.
Wong said children who get the flu need to be watched carefully. She recommends getting in touch with the child’s doctor when symptoms start.
“That’s especially true for kids with high-risk medical conditions and for very young children,” she explained. “These children are at especially high risk for flu complications.”
Laufer, however, said a phone call to the doctor isn’t enough. “It’s very difficult for a pediatrician on the other side of the phone to understand how sick the child really is,” he said.
Parents should take their child to the doctor or emergency department if they’re sicker than what one would expect with a common cold, he said.
“Parents should realize that influenza is much more than sniffles,” Laufer added. “A kid with influenza is a kid who is very sick, is a kid who is lethargic, has decreased appetite, is not drinking as much and not urinating as much in addition to other flu symptoms,” he said.
Wong added that early antiviral treatment is recommended for high-risk children who develop symptoms of influenza. “That’s another thing they can talk to their health care provider about,” Wong added.
Antiviral drugs include Tamiflu, Relenza, Symmetrel and Flumadine.
In the study, Wong’s group found that of the 794 children whose medical history was known, 43 percent had no medical condition that put them at high risk of dying from flu.
As for children with high-risk medical conditions who died, 33 percent had neurological conditions such as cerebral palsy or seizure disorder, and 12 percent had a genetic condition that put them at risk for flu complications.
Asthma, lung disease, heart disease and cancer can also increase a child’s odds of dying from flu, the researchers noted.
Each year in the United States, flu causes an estimated 54,000 to 430,000 hospitalizations and 3,000 to 49,000 deaths, with infection rates highest among children, according to the CDC.










