 Medical school applications and enrollment reached record highs this year as organized medicine’s cries for more funding for residency slots continued with little response from Congress.
Medical school applications and enrollment reached record highs this year as organized medicine’s cries for more funding for residency slots continued with little response from Congress.
The number of first-year medical students exceeded 20,000 for the first time in 2013, reaching 20,055, the Association of American Medical Colleges (AAMC) said Thursday in its annual report on medical school enrollment and applications.
Meanwhile, first-year student enrollment at osteopathic medical colleges increased 11.1% in 2013, to 6,449, according to the American Association of Colleges of Osteopathic Medicine (AACOM).
The two organizations increased their pleas for Congress to provide more money for graduate medical education and funding residency training slots to handle the newly minted doctors.
“We think, that as much as we see gridlock in Washington, that is something that we need to attend to sooner rather than later,”Atul Grover, MD, PhD, chief public policy officer at AAMC, said during a congressional briefing Thursday.
First-time medical school enrollment jumped 2.8% this year and is up 21.6% since 2002, according to the AAMC. The group attributed the increase to four medical schools opening their doors this year and an additional 14 increasing their class sizes by more than 10%.
Total medical school applications are up 6.1% to 48,014, this year while first-time applicants have grown 5.8%, the AAMC said. First-time female applicants increased 6.9%, after remaining flat in 2012. Hispanics attendance at medical schools increased 5.5%.
Furthermore, total enrollment at osteopathic medical schools increased to 4.9% over 2012, growing to more than 22,000 students. New osteopathic medical schools opened in the last year in Alabama, North Carolina, and Indiana.
“Because large numbers of new osteopathic physicians become primary care physicians, often in rural and underserved areas, it is evident that the osteopathic medical profession will help the nation alleviate a primary care physician crisis,” Stephen Shannon, DO, MPH, AACOM president and chief executive, said in a statement. “And colleges of osteopathic medicine are expanding and increasing to meet this demand.”
But the increase in enrollment will mean little in the fight to ease the nation’s physician shortage unless teaching hospitals have a greater ability to train physicians, the AAMC and AACOM said. The AAMC projects a shortage of more than 90,000 doctors by 2020.
“Unless Congress lifts the 16-year-old cap on federal support for residency training, we will still face a shortfall of physicians across dozens of specialties,” AAMC President and Chief Executive Darrell Kirch, MD, said in a release. “Students are doing their part by applying to medical school in record numbers. Medical schools are doing their part by expanding enrollment. Now Congress needs to do its part and act without delay to expand residency training to ensure that everyone who needs a doctor has access to one.”
The Balanced Budget Act of 1997 limited the number of residencies Medicare would support. But seeing the pending shortage of physicians coming, the AAMC pleaded with its members in 2006 to increase its enrollment, which was mostly flat between 1980 and 2006.
While medical schools have complied, the number of residency training positions has remained the same. Nearly 1,000 graduates initially were unmatched last year, a number that was eventually whittled down to 520.
“We should probably be training another 4,000 doctors per year,” Grover said.
With 26,504 medical students starting in 2013 between osteopathic and allopathic medical schools, only 26,392 first-year residency slots existed in 2013, Grover said.
“We hear from our educators and our teaching hospitals the way that clinical revenues have been compressed, they don’t have the resources for additional positions anymore,” he added.
Legislation is pending in both chambers — H.R. 1201 and S. 577 — that would increase the number of residency slots Medicare would support by 15,000 over 5 years. The legislation would cost about $9 billion over 10 years, Grover said.
It costs about $145,000 a year to train a physician, but Medicare supports only about $3.2 billion annually of the roughly $15 billion it takes to train physicians nationwide.
Source: Med Page today





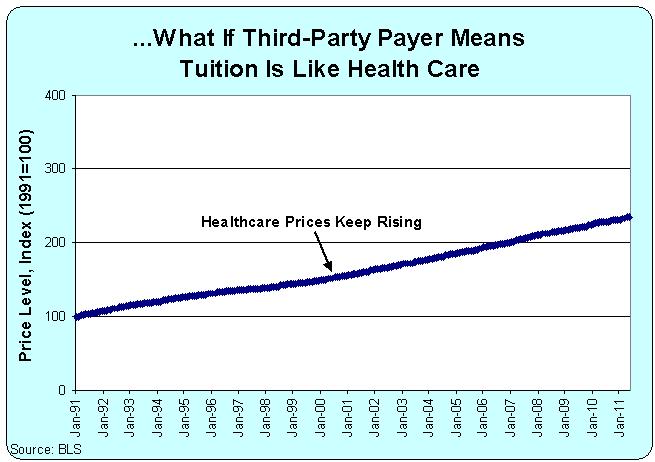 “In the case of medical education, students buy their education from medical schools and resell that education in the form of services to patients. Medical education can remain expensive only so long as there are patients, insurers, and employers who are willing to pay high prices for health care. But if prices for physician services decline, then the cost of medical education will have to decline too, or people won’t be willing to pay for medical school in the first place,” Asch says.
“In the case of medical education, students buy their education from medical schools and resell that education in the form of services to patients. Medical education can remain expensive only so long as there are patients, insurers, and employers who are willing to pay high prices for health care. But if prices for physician services decline, then the cost of medical education will have to decline too, or people won’t be willing to pay for medical school in the first place,” Asch says.


 Medical school applications and enrollment reached record highs this year as organized medicine’s cries for more funding for residency slots continued with little response from Congress.
Medical school applications and enrollment reached record highs this year as organized medicine’s cries for more funding for residency slots continued with little response from Congress.
 Dr Hossien spent over six months developing his invention A heart surgeon at a Swansea hospital has won an award for an invention that cost him 95p to create. Morriston hospital doctor Abdull razak Hossien made his surgery training simulator out of a sweet tin. The portable device can be used anywhere and is now being manufactured for use around the world
Dr Hossien spent over six months developing his invention A heart surgeon at a Swansea hospital has won an award for an invention that cost him 95p to create. Morriston hospital doctor Abdull razak Hossien made his surgery training simulator out of a sweet tin. The portable device can be used anywhere and is now being manufactured for use around the world


 Low treatment costs and high levels of expertise have made India a leading destination for heart treatment for people from West Asian and African countries, doctors said.
Low treatment costs and high levels of expertise have made India a leading destination for heart treatment for people from West Asian and African countries, doctors said.