Brain cancer can play a deadly game of hide and seek.
A new study published in the journal Science has revealed that brain cancer cells can actually evade many current cancer drugs – by temporarily scaling down a certain genetic mutation that the drugs target. Additionally, once therapy has stopped, the cancer cells can then intensify the mutation once again.
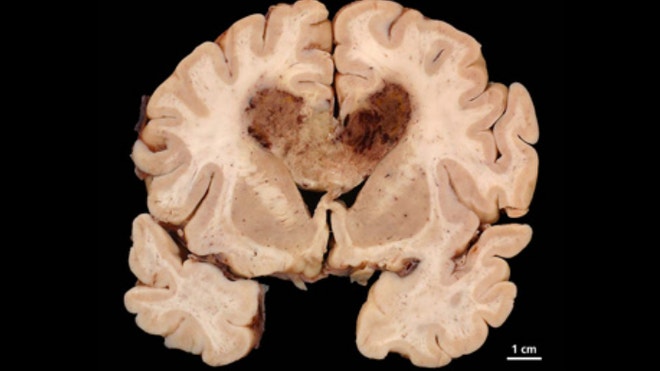
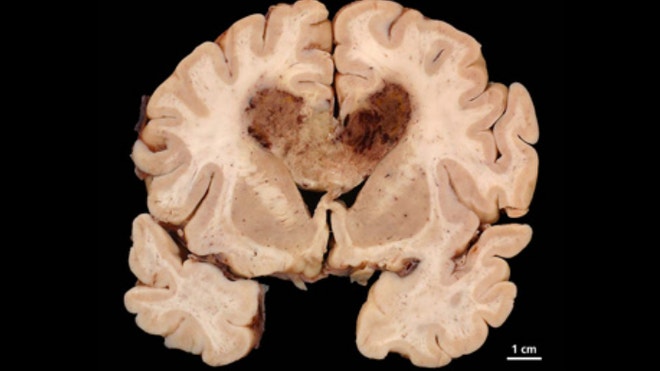
According to the researchers, this study has huge implications for the future treatment of glioblastoma multiforme (GBM) – a brain cancer that is in desperate need of effective therapies.
“It’s one of the most common types of adult brain cancer and one of the most lethal of all types of human cancers,” study author Dr. Paul Mischel, a member of the Ludwig Institute for Cancer Research and a professor in the department of pathology at the University of California, San Diego, told FoxNews.com. “And there are a number of real challenges [in treatment]. There are no good early detections for the disease, and the tumor cells invade through the brain, so it’s almost completely impossibly to surgically remove the entire tumor.”
Mischel also noted that GBM becomes resistant to modern chemotherapy and radiation treatments relatively quickly.
Recently, alternative cancer drugs have emerged that are capable of targeting specific genetic mutations in cancer cells. About 60 percent of GBM cells express a mutated variant of the epidermal growth factor receptor – also called EGFRvIII. Found in the extrachromosomal DNA of these cancer cells, EGFRvIII helps to promote tumor growth and proliferation, and many targeted therapies work by targeting and suppressing this specific mutation.
However, these drugs ultimately haven’t translated to better outcomes for GBM patients.
“You would think that drugs that are used to target that receptor would be effective, but the results have been very disappointing,” Mischel said.
In order to better understand why, Mischel and his research team analyzed the genetic makeup of GBM tumors. When they treated the cancer cells with targeted therapies, they found that the pieces of mutant EGFRvIII DNA, which normally float outside the cancer’s chromosomes, temporarily jumped onto an obscure chromosome — where they could “hide” from the drugs. Then, once they ceased treatment, the DNA pieces removed themselves from the chromosome and floated freely once again, promoting cancer cell proliferation.
So in essence, the cancer cells were able to “shut down” the expression of the mutation while the cancer drugs were present in the body.
“This was a real surprise,” Mischel said. “…Those pieces of extra chromosomal DNA ‘disappeared’ when treated with the drug. It’s truly a hide-and-seek mechanism, because when the drug was removed, it jumped back off the chromosome.”
Mischel said it is still not understood exactly how the cancer can detect the presence of the drugs in the body, but the researchers have a few preliminary ideas.
“The mechanism by which the DNA is sensing the drug is really not understand,” Mischel said. “But the theory is that the DNA is sensing the signals that are being sent indirectly by the drug.”
The study’s findings help better explain why GBM becomes resistant to targeted therapies and it may help doctors determine a better course of treatment for patients. Mischel argued that the discovery could completely change how physicians treat patients with other types of cancer as well.
“It’s really a complete paradigm shift in how we begin to think about treating people with targeted therapies,” Mischel said. “…This find has big implications for this disease, because other types of cancers have these mutations present on extra chromosomal DNA….How we dose these tumors could change. The data we have in hand would suggest a very different type of dosage for targeted cancer treatment.”
Source: all voices