Scientists at A*STAR’s Institute of Molecular and Cell Biology (IMCB) have developed a method to generate human induced pluripotent stem cells (hiPSCs) from a single drop of finger-pricked blood.
The method also enables donors to collect their own blood samples, which they can then send to a laboratory for further processing. The easy access to blood samples using the new technique could potentially boost the recruitment of greater numbers and diversities of donors, and could lead to the establishment of large-scale hiPSC banks.
By genetic reprogramming, matured human cells, usually blood cells, can be transformed into hiPSCs. As hiPSCs exhibit properties remarkably similar to human embryonic stem cells, they are invaluable resources for basic research, drug discovery and cell therapy.
In countries like Japan, USA and UK, a number of hiPSC bank initiatives have sprung up to make hiPSCs available for stem cell research and medical studies.
Current sample collection for reprogramming into hiPSCs include invasive measures such as collecting cells from the bone marrow or skin, which may put off many potential donors. Although hiPSCs may also be generated from blood cells, large quantities of blood are usually required.
In a paper published in Stem Cells Translational Medicine, scientists at IMCB showed for the first time that single-drop volumes of blood are sufficient for reprogramming into hiPSCs. The finger-prick technique is the world’s first to use only a drop of finger-pricked blood to yield hiPSCs with high efficiency. A patent has been filed for the innovation.
The accessibility of the new technique is further enhanced with a DIY sample collection approach. Donors may collect their own finger-pricked blood, which they can then store and send it to a laboratory for reprogramming.
The blood sample remains stable for 48 hours and can be expanded for 12 days in culture, which therefore extends the finger-prick technique to a wide range of geographical regions for recruitment of donors with varied ethnicities, genotypes and diseases.
By integrating it with the hiPSC bank initiatives, the finger-prick technique paves the way for establishing diverse and fully characterised hiPSC banking for stem cell research.
The potential access to a wide range of hiPSCs could also replace the use of embryonic stem cells, which are less accessible. It could also facilitate the set-up of a small hiPSC bank in Singapore to study targeted local diseases.
Loh Yuin Han Jonathan, principal investigator at IMCB and lead scientist for the finger-prick hiPSC technique, said, “It all began when we wondered if we could reduce the volume of blood used for reprogramming. We then tested if donors could collect their own blood sample in a normal room environment and store it. Our finger-prick technique, in fact, utilised less than a drop of finger-pricked blood. The remaining blood could even be used for DNA sequencing and other blood tests.”
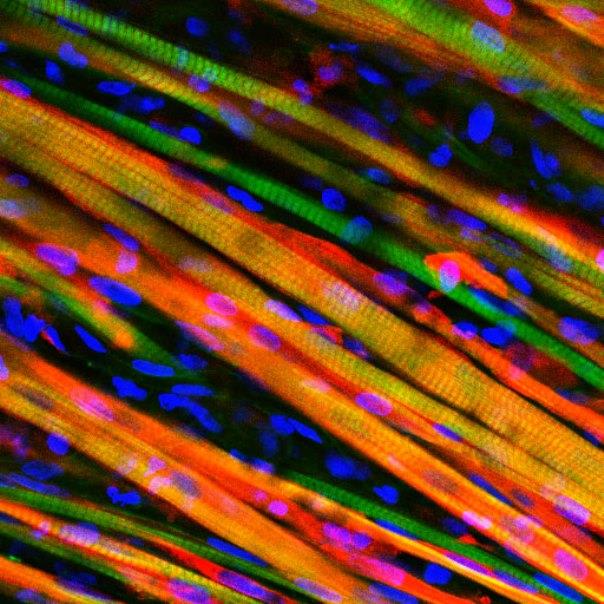
Stuart Alexander Cook, senior consultant at the National Heart Centre Singapore and co-author of the paper, said, “We were able to differentiate the hiPSCs reprogrammed from Jonathan’s finger-prick technique, into functional heart cells. This is a well-designed, applicable technique that can unlock unrealized potential of biobanks around the world for hiPSC studies at a scale that was previously not possible.”
Hong Wanjin, executive director at IMCB, said, “Research on hiPSCs is now highly sought-after, given its potential to be used as a model for studying human diseases and for regenerative medicine. Translational research and technology innovations are constantly encouraged at IMCB and this new technique is very timely. We hope to eventually help the scientific community gain greater accessibility to hiPSCs for stem cell research through this innovation.”
Source: India medical Times



 Researchers have found that in boys, higher screen time was adversely associated to bone mineral density (BMD) at all sites even when adjusted for specific lifestyle factors.
Researchers have found that in boys, higher screen time was adversely associated to bone mineral density (BMD) at all sites even when adjusted for specific lifestyle factors.