At any healthcare centre, the most common form of intervention recommended for a patient by a physician is drug therapy. Things go awry when medications are wrongly administered for reasons that could be lack of professional practice or other unintentional human errors, incompetent healthcare products and lax procedures and systems. Observational studies all over the world have identified that errors associated with medications are the most frequent cause of adverse medical events.
Erroneous drug administration though, unfortunately, under-reported remains a rampant iatrogenic induced insult to patients. Medical errors are known to be the leading cause of death in the US and probably worldwide. A total of 44,000-98,000 Americans die every year due to this. It’s estimated that each year medical errors injure at least 1.5 million Americans and cost the health system more than 3.5 billion US dollars. Many anaesthesiologists have faced legal prosecution for allegations ranging from malpractice to homicide.
The major consequences of erroneous intravenous drug administration are patient’s morbidity and mortality that could cause a great psychological pain to patients, families, and healthcare providers. Prolonged hospital stay can increase financial burden on patient and healthcare system besides eroding public confidence and trust in healthcare services.
To prevent potential errors during drug administration, a technological innovation by Dr Anurag Tewari, a Fellow of neurosurgical and spine anaesthesiologist at US-based Cleveland Clinic Foundation, could provide a possible solution to minimize medication related errors.
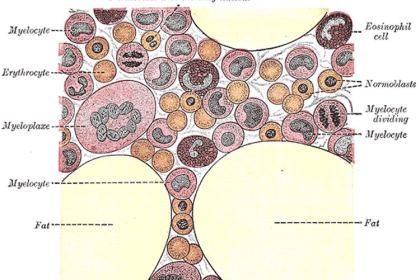
Dr Tewari has designed an innovative drug delivery system called VEINROM, which could totally obliterate the incidence of wrong drug administration in anaesthesiology and other critical care areas. VEINROM (an acronym for Vasopressors, Emergency medicine, Induction agents, Neuromuscular blockers, Reversal drugs, Opioids/painkillers and Miscellaneous drugs) has been proposed by him as a conceivable solution to erroneous intravenous drug administration. The above seven categories of drugs encompass most of the intravenous drugs that are used frequently in anaesthesia.
The envisioned fluid delivery system, VEINROM, will harbour one syringe port for each of the seven drug class categories that are most commonly used drugs in anaesthesiology and critical care. A deterrent to prevent erroneous drug administration, VEINROM is a unique drug delivery manifold and syringe assembly which has incorporated mechanical and electronic mechanisms that will make it very difficult to administer wrong drugs intravenously. Preloaded syringes will further decrease the potential for human error when administering drugs instead of loading-labelling them perioperatively.
The report has been published in the Journal of Anaesthesiology Clinical Pharmacology.
Dr Tewari told India Medical Times, “VEINROM is so far the safest and the only fail-proof intravenous drug delivery assembly of specialized syringes and manifold. It incorporates more than six deterrents that will obliterate the chance of a physician injecting wrong drug into the patient.”
“This is definitely a path breaking innovation in anaesthesiology, critical care and emergency medicine. All three fields are related to service providers working under extreme duress, which predisposes them to inadvertently inject wrong drug into patient’s blood stream. VEINROM intends to ameliorate this potentially lethal outcome and hence circumvent patient harm and also malpractice lawsuits against physicians worldwide,” he added.
Instrumental in designing the technology, Dr Tewari also collaborated with four senior students of the biomedical engineering department of the University of Iowa, US on conceptualizing and designing the prototypes of VEINROM as per the ASTM (American Standards Testing Materials) regulations.
“The four students were Taylor Hines, Brady Palm, Trace Royer, and Eric Alexander. Project VEINROM was adjudged as the best senior research project by the university, besides being awarded prestigious prizes in Francis Elevator Pitch and Huber Storer Entrepreneurial competitions. Right now we are promoting this concept to various manufacturers hoping its introduction into practice will soon lead to enhanced patient safety,” he said.
About his plans to bring the technology to India, Dr Tewari said, “I hope to reach out to the country’s medical fraternity to incorporate this into their practice and help patients and themselves via media. The incidence of erroneous drug administration in India is perhaps equal or more than in the developed nations. Countrymen and physicians stand to benefit immensely from VEINROM.”
Many a times, some of the best people make the worst mistakes and even the best systems sometimes fail to prevent recurring medical errors. Perhaps, it’s the time to bring some changes in the field of anaesthesiology and modification in the safety protocol is essential. Adoption of best practices along with innovative technology could potentially minimize medical errors and improve overall healthcare system and most importantly save lives.
Source: India Medical Times