
If you haven’t heard about the threat “superbugs” (bacteria that are resistant to antibiotics) pose to our health, it’s likely you haven’t been conscious or on the planet for a couple of years.
There are no new drugs in the pipeline to fix the superbug problem. And when times are tough, and we’re faced with life-threatening infections, we often turn to alternative, sometimes unproven methods.
Research recently published in The Lancet looked at whether applying medical grade honey to wound sites in patients undergoing dialysis showed advantages over standard antibiotic use.
We are susceptible to bacterial infection whenever our skin is punctured, which happens quite a lot during hospital treatment. The researchers worked with dialysis patients because having a catheter inserted is a regular procedure for the hundreds of thousands of kidney dialysis patients.
They found that using honey showed no advantages over standard antibiotic use, and was, in fact, worse for diabetic dialysis patients.
Getting something like honey to the market as a food product is pretty straightforward, but for medicines the bar is set higher.
The drug approval process
There are many different ways that new medicines are approved for public use.
Drugs made by pharmaceutical companies, for instance, go through many years of expensive, highly-controlled clinical trials comparing the effects of the new drug against a placebo control. And later, they are compared against competitor compounds already on the market.
But alternative, or “natural” medicines can be put straight to market provided they don’t do any harm and their makers don’t make outrageous claims about their health effects.
One such natural alternative is bee honey, which has long been known to have antibacterial activity. A commercial version of “antibiotic” honey, Medihoney, has actually been clinically evaluated for the treatment of ulcers.
Honey is cheap and widely available, and while it cannot be used for systemic infections (for pneumonia, for instance, or bacteremia), it has been used for open wounds. It can kill many types of bacteria and is thought also to provide a barrier to moisture.
The bake off
The Lancet paper looked closely at how a naturally-derived honey preparation compares against a clinically-approved antibiotic – a drug called Bactroban that’s used to kill bacteria found in and around wounds.
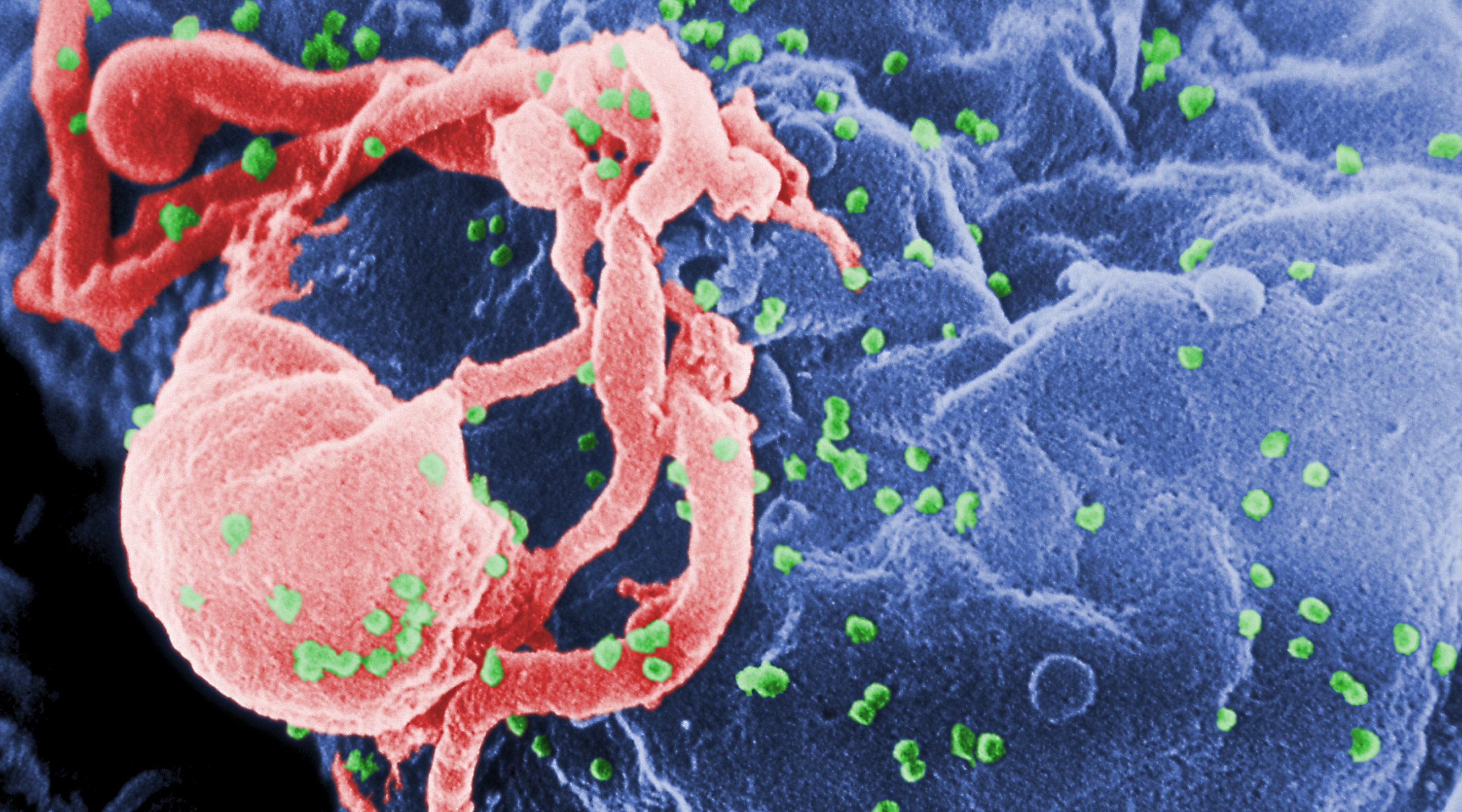
The main culprit, Staph aureus, lives on our skin and can cause infection around catheters used during treatment of dialysis-related infections.
A total of 371 trial participants undergoing dialysis received either standard antibiotic therapy to prevent infection, or a daily application of medical grade honey, to the site of catheter insertion.
The study found no significant differences in infection rates or deaths from infection between most people given the antibiotic or people given honey.
But for people with diabetes, which is often associated with kidney disease, the honey actually increased the risk of infection. This is important because diabetes is the leading cause of kidney failure, so any therapy should work with normal and diabetic kidney dialysis patients.
The reasons for the diabetes-kidney failure link are not completely understood, but diabetics often have both high blood glucose levels and high blood pressure, both of which can cause kidney damage.
There’s also a hormone system called the renin-angiotensin system that regulates blood pressure and fluid balance involving the kidney, which is unbalanced in diabetics.
While honey therapy was worse than antibiotics for diabetics, the authors found the most important factor for preventing infection in all patients was how well the catheter was inserted and fixed. There was no placebo control possible in the trial (where no treatment is given) as these infections are sometimes fatal.
We can conclude that honey therapy instead of antibiotics at least does no harm for many dialysis patients, but also that it’s not good for diabetics. And because diabetes and kidney disease are commonly linked and 9% of the patients treated with either therapy still died, the bottom line is still that we need better therapies for bacterial infection – whether natural or man-made.









 Animals have aided the blind for quite some time now. More recently, they have been trained to help calm children with autism and detect health conditions like cancer and diabetic episodes. However, there’s little evidence to indicate that dogs can actually detect epileptic seizures. But you couldn’t tell an Irish family that. They say that Charlie, their Great Dane, can detect their daughter’s epileptic fits before they happen.
Animals have aided the blind for quite some time now. More recently, they have been trained to help calm children with autism and detect health conditions like cancer and diabetic episodes. However, there’s little evidence to indicate that dogs can actually detect epileptic seizures. But you couldn’t tell an Irish family that. They say that Charlie, their Great Dane, can detect their daughter’s epileptic fits before they happen. The study showed the vaccine had a protective efficacy of 65 percent over a five-year period.
The study showed the vaccine had a protective efficacy of 65 percent over a five-year period.