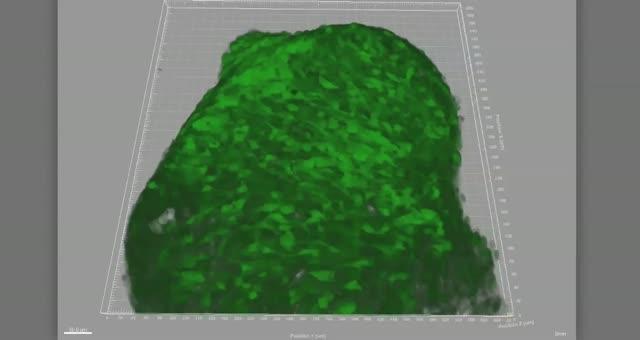
Scientists were astonished to find they could predict which healthy people are at most risk of death by studying four key biomarkers in the body
A ‘Death Test’ which predicts the chance of a healthy person dying from any medical condition in the next five years has been developed by scientists.
Researchers said they were ‘astonished’ to discover that a simple blood test could predict if a person was likely to die – even if they were not ill.
They found that the levels of four ‘biomarkers’ in the body, when taken together, indicated a general level of ‘frailty’.
People whose biomarkers were out of kilter were five times more likely to die with five years of the blood test.
“What is especially interesting is that these biomarkers reflect the risk for dying from very different types of diseases such as heart disease or cancer. They seem to be signs of a general frailty in the body,” said Dr. Johannes Kettunen of the Institute for Molecular Medicine in Finland.
“We believe that in the future these measures can be used to identify people who appear healthy but in fact have serious underlying illnesses and guide them to proper treatment.”
A biomarker is a biological molecule found in blood, body fluids, or tissues that may signal an abnormal process, a condition, or a disease.
The level of a particular biomarker may indicate a patient’s risk of disease, or likely response to a treatment. For example, cholesterol levels are measured to assess the risk of heart disease.
Most current biomarkers are used to test an individual’s risk of developing a specific condition. There are none that accurately assess whether a person is at risk of ill health generally, or likely to die soon from a disease.
Blood samples from over 17,000 generally healthy people were screened for more than a hundred different biomarkers and those people monitored over five years
In that time 684 people died of a range of illnesses and diseases, including cancer and cardiovascular disease. Scientists discovered that those people all had similar levels of four biomarkers.
Those were albumin, alpha-1-acid glycoprotein, citrate and the size of very-low-density lipoprotein particles which are linked to liver and kidney function, inflammation and infection, energy metabolism and vascular health.
One in five participants with the highest biomarker scores died within the first year of the study.
Estonian researchers made the initial link in a cohort of 9,842 people but were so sceptical about the results that they asked Finnish scientists to repeat the experiment on a further 7,503.
Research professor Markus Perola of the Institute for Health and Welfare, Finland said they were not expecting to be able to replicate the findings and were amazed when they were identical.
Prof Perola said: “It was a pretty amazing result. First of all we didn’t really believe it. It was astonishing that these biomarkers appeared to actually predict mortality independent of disease.
“These were all apparently healthy people but to our surprise it appears these biomarkers show an undetected frailty which people did not know they had.”
Researchers claim that in the future a test could flag up high-risk individuals in need of medical intervention who show no symptoms of any disease.
“If the findings are replicated then this test is surely something we will see becoming widespread,” added Prof Perola.
“But at moment there is ethical question. Would someone want to know their risk of dying if there is nothing we can do about it?”
Dr Kettunen added: “Next we aim to study whether some kind of connecting factor between these biomarkers can be identified.
Source: Telegraph